Digestive Problems and Menopause: What the Heck Is Going On with Your Gut?
Experiencing more digestive problems lately? Wondering if they could be related to menopause?
For many women, the changes are sudden and hard to ignore—heartburn that burns long after meals, bloating that makes your waistband dig in, or bowel habits that swing from one extreme to the other.
As a registered dietitian specializing in menopause nutrition, I know how disruptive it can be. Let’s look at some of the most common digestion changes in midlife, why they happen, and practical ways to get relief.
How Hormonal Changes Affect Digestion
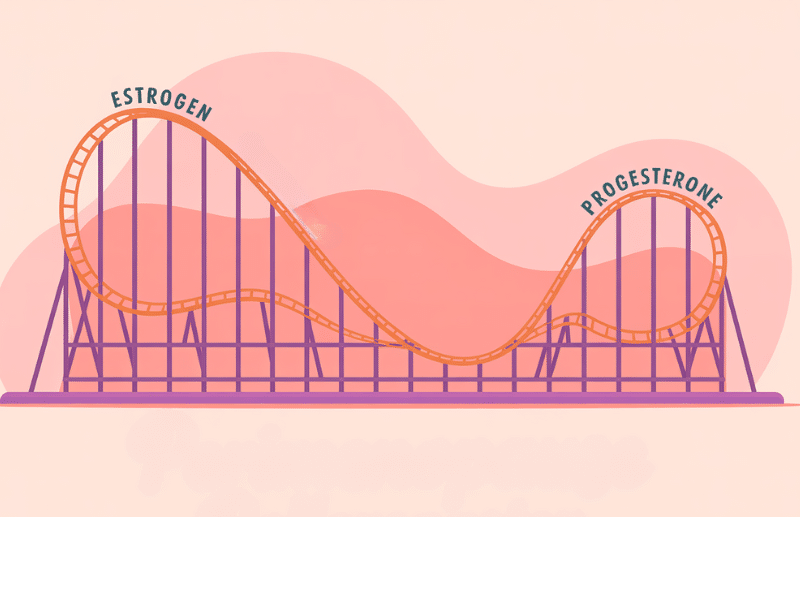
During perimenopause estrogen and progesterone levels begin to fluctuate and eventually decline. These hormonal shifts can influence the digestive system in a few key ways:
Slower movement through the gut: Lower progesterone can slow intestinal muscle contractions, meaning food takes longer to pass through. This can contribute to constipation, bloating or a feeling of heaviness after meals.
Changes in bile production: Estrogen helps regulate bile secretion, which aids in digesting fats. When estrogen drops, bile production can decrease, making fatty meals harder to tolerate and increasing the risk of bloating or indigestion.
Gut microbiome shifts: Hormonal changes can alter the balance of bacteria in the gut, which may affect digestion, immunity, and even inflammation levels.
Increased gut sensitivity: Hormone fluctuations can heighten the nervous system’s response to normal digestive activity, making you more aware of bloating, cramps, or discomfort.
Common Perimenopause Stomach Issues
Digestive changes in midlife don’t always follow a clear pattern. Some women notice just one persistent issue, while others cycle through different symptoms over time.
Digestive Symptom Tracker for Midlife Women
A simple tool to help you spot patterns, uncover
triggers, and feel better in your body.
Start tracking today and finally feel in control.
Here are the most common digestive issues I see:
Heartburn/Acid Reflux/GERD

What it is: A burning sensation in the chest or throat, often after eating, sometimes with a sour taste in the mouth.
Why it happens in menopause: Lower estrogen and progesterone can relax the lower esophageal sphincter (the muscle that keeps stomach acid where it belongs), making reflux more likely. A slower digestive process and midlife lifestyle factors can add to the problem.
Quick relief tips:
- Eat smaller, more frequent meals: Large meals put more pressure on the stomach and can trigger reflux.
- Identify and limit trigger foods: Common culprits include tomatoes, citrus fruits, coffee, alcohol, chocolate, and carbonated drinks—though yours may differ. Keeping a food diary can help.
- Stay upright after eating: Wait at least an hour before lying down and avoid eating too close to bedtime.
- Elevate your upper body at night: Sleeping on a slight incline can reduce nighttime heartburn.
Read more in my full article: Menopause Heartburn Relief
Constipation

What it is: Infrequent bowel movements (fewer than three per week), hard stools, or straining during bowel movements.
Why it happens in menopause: Progesterone slows intestinal muscle contractions, and declining estrogen may affect hydration in the gut. Reduced activity levels, lower fiber intake, and certain medications can make it worse.
Quick relief tips:
- Increase fiber gradually: Add more fruits, vegetables, whole grains, and legumes over time to prevent worsening bloating or discomfort.
- Stay well-hydrated: Adequate fluids help soften stools and support healthy digestion.
- Move daily: Even short walks can help stimulate bowel motility.
- Go when you feel the urge: Delaying can make stools harder and more difficult to pass.
Read more in my full article: Menopause and Constipation
Diarrhea

What it is: Loose or watery stools that occur more frequently than normal.
Why it happens in menopause: Hormone fluctuations can affect the gut’s muscle contractions and sensitivity, sometimes speeding things up. Stress, dietary triggers, and gut microbiome changes can also play a role.
Quick relief tips:
- Add soluble fiber gradually: Foods like oats, barley, carrots, and sweet potatoes can help absorb excess water in the gut and improve stool consistency.
- Identify and limit trigger foods: Common culprits include lactose, certain fruits, alcohol, and fatty meals. Keeping a short-term food diary can help.
- Stay hydrated: Replace fluids with water, herbal tea, or broths to avoid dehydration.
- Consider probiotics: Yogurt, kefir, or fermented vegetables may help support a balanced gut microbiome.
Read more in my full article: Menopause and Diarrhea
Bloating

What it is: A feeling of fullness, tightness, or swelling in the abdomen, sometimes with gas or discomfort.
Why it happens in menopause: Hormonal changes can slow digestion, affect fluid balance, and make the gut more sensitive to certain foods. Constipation, fluid retention, and stress can also contribute.
Quick relief tips:
- Stay hydrated: Water helps keep digestion moving and can reduce fluid retention.
- Limit sodium from packaged foods: Too much salt can increase water retention and bloating.
- Increase fiber slowly: Adding high-fiber foods gradually can prevent gas while supporting regularity.
- Identify personal trigger foods: Common culprits include beans, certain vegetables, fizzy drinks, and dairy.
- Move after meals: A short walk can help release trapped gas and stimulate digestion.
Read more in my full article: Menopause and Bloating
When to Seek Medical Advice

While digestive changes are common in menopause, some symptoms deserve prompt attention from a healthcare provider. Seek medical advice if you experience:
- Unexplained weight loss
- Blood in your stool or black/tarry stools
- Persistent or severe abdominal pain
- Frequent vomiting or nausea
- Changes in bowel habits lasting more than a few weeks
- Ongoing diarrhea or constipation that doesn’t improve with simple changes
Keeping track of your symptoms can help both you and your healthcare provider spot patterns and determine the best next steps.
I’ve created a Menopause Digestive Symptom Tracker you can use to record what you’re experiencing, when it happens, and any potential food or lifestyle triggers.
Download your Free Symptom Tracker
Digestive problems in menopause can range from mildly annoying to downright disruptive. While they may be linked to normal hormonal changes, that doesn’t mean you have to simply put up with them. Small, consistent changes to diet, hydration, and daily habits can make a noticeable difference.

Looking for ongoing support around food, body, and menopause?

Hi, I’m Sandra!
I’m a registered dietitian and body confidence coach specializing in midlife health and menopause nutrition.
I help women thrive by moving away from restriction and toward nourishment—through practical strategies and compassionate support that honor your changing body.
My focus is on helping you feel confident, strong, and well-fed.
Learn more






