Menopause Bloating: What Causes It and How to Stop It
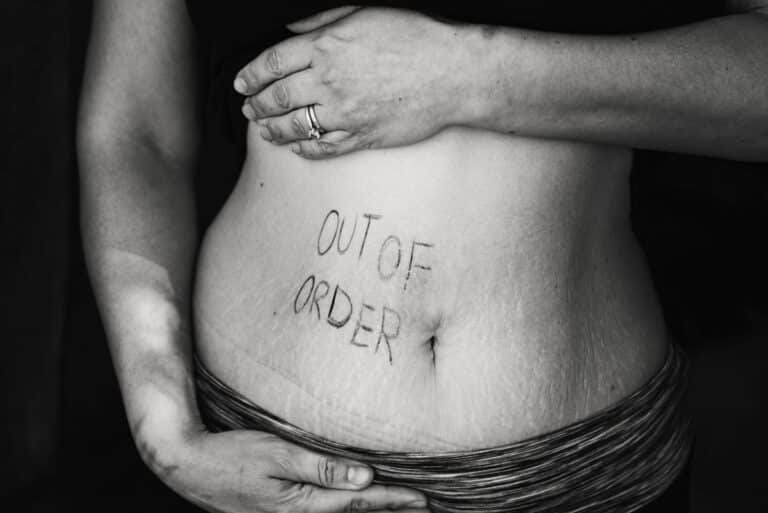
Feeling bloated during menopause?
It’s one of those sneaky symptoms no one really warns you about — until you’re suddenly living it. You wake up feeling fine, but by mid-afternoon, your waistband feels like it’s plotting against you. Bloating during menopause is surprisingly common, and for many of us, it’s more than just an occasional nuisance.
Let’s unpack what’s going on — and more importantly, what you can actually do to feel better.
What does menopause bloating feel like?

I hear from so many women about the dreaded “meno-belly.” But let’s clear something up — there’s a difference between the natural body composition changes of midlife (hello, extra padding around the middle) and true bloating.
Weight gain around your midsection might make your jeans a bit snug, but it’s not the same as that ballooned-up, can’t-wait-to-unbutton-my-pants sensation bloating brings.
Common symptoms of perimenopausal bloating:
- A feeling of fullness or tightness in your abdomen
- A visibly rounded or distended stomach
- More burping than you’d like to admit
- Increased gas(awkward, I know)
For some women, bloating is a constant companion. For others, it creeps up slowly through the day — flat belly at breakfast, beach ball by bedtime. Certain meals might trigger it, or it might hang around for days at a time. And yes, it can absolutely interfere with your quality of life.
Here’s a fascinating wrinkle: research shows this isn’t a universal experience. A 2021 study found that Asian women reported fewer and less severe gastrointestinal symptoms during the menopause transition compared to non-Hispanic white women.
Why? That’s still being explored, but it’s a reminder that our menopause journeys can look — and feel — very different.

Why does bloating happen in perimenopause?

During perimenopause, estrogen and progesterone levels can rise and fall unpredictably — sometimes within the same week, sometimes the same day. Those hormonal swings have a surprisingly big impact on your digestion and how your body handles fluids. Here’s what can happen:
1. Increased water retention
When your body holds onto more fluid, it can show up as swelling in your hands, ankles… and yes, your abdomen. That puffiness is often a mix of hormonal changes and sodium (salt) intake.
Estrogen plays a key role in regulating body fluids — it even affects your thirst, how much water you drink, and your salt cravings. Meanwhile, progesterone normally acts like a natural diuretic, helping your body flush out extra fluid. But as progesterone drops, your body is more likely to hang onto water, adding to that bloated feeling.
Fun fact (or maybe not-so-fun): A 2020 study found that eating a lot of sodium can make this worse, so salty snacks might be adding to the bloat.
2. Decreased bile production
Estrogen and progesterone influence bile production — and bile is like a natural lubricant for your intestines, helping you digest fats efficiently. When bile production slows down (thanks to higher estrogen and lower progesterone), your digestion can feel sluggish. Less bile means fats aren’t broken down as well, and that can leave you feeling heavier and more bloated after meals.

3. Slowed digestion
Both estrogen and progesterone affect peristalsis — that gentle, rhythmic movement that pushes food through your gut. When estrogen levels zigzag, gut motility slows, and food lingers longer than it should. This can lead to constipation, a lingering feeling of fullness, and more opportunity for gas to build up.
4. Increased intestinal gas
Speaking of gas — it’s not just about food moving slowly. Menopause can also shift the balance of bacteria in your gut (your microbiome). These tiny microbes help digest food, but when their balance changes, you can end up with more gas production. And if your gut is moving slowly? That gas hangs around longer, adding to the pressure.
5. Increase pain sensitivity
Hormonal fluctuations can make your digestive organs more sensitive to discomfort. That means bloating that once barely registered can now feel like a major event. You’re not imagining it — your gut is literally more reactive during this stage of life.
Treatment for menopausal bloating

Taming menopause bloating can be a bit of detective work — it’s all about figuring out why it’s happening for you, then targeting that cause. Here are strategies and lifestyle tweaks that can help:
1. Stay hydrated.
It might sound counterintuitive, but drinking more water can actually help reduce bloating — especially if it’s caused by fluid retention. Adequate hydration keeps your digestive system moving, reduces constipation, and helps flush excess sodium from your body.
Aim for around 8 cups a day. Hormone changes can dull your natural thirst cues, so don’t just wait to feel thirsty. Keep water nearby and sip throughout the day.
Check out how Staying Hydrated Can Help You Feel Better During Menopause
2. Reduce your salt.

Too much sodium encourages your body to hold onto water. More than 70% of the sodium we eat comes from packaged foods, not the saltshaker, so label-reading can make a big difference.
As a registered dietitian, I recommend keeping daily sodium intake between 1,500–2,000 mg. For flavor without salt, try lemon juice, vinegar, or experiment with spices and herbs (I often double them in recipes for more punch).
3. Increase fiber-slowly.
Fiber supports healthy digestion and can prevent constipation, but jumping from low to high fiber overnight can make bloating worse. Increase gradually: add one high-fiber food or meal, wait to see how you feel, then add more.

Check out this FREE printable list of high fiber foods.
Don't miss out on the other benefits from fiber during menopause.
4. Identify trigger foods.
Our digestion changes with menopause, and foods that never bothered you before might suddenly cause gas or bloating.
I routinely suggest that my clients keep a food journal to help them sort out exactly what might be causing their discomfort. Foods you previously ate with no problem may now be giving you grief. Some people may be more sensitive to certain foods that can cause gas.
Digestive Symptom Tracker for Midlife Women
A simple tool to help you spot patterns, uncover
triggers, and feel better in your body.
Start tracking today and finally feel in control.
Food that can cause gas:
- Beans (Presoaking reduces the gas-producing potential of beans if you discard the soaking water and cook using fresh water)
- Vegetables such as artichokes, asparagus, broccoli, cabbage, Brussels sprouts and cauliflower.
- Whole grains and bran (Adding them slowly to your diet can help reduce gas forming potential)
- Fizzy drinks
- Milk and milk products, such as cheese and ice cream
- Foods containing sorbitol, such as sugar-free candies and gums
Be very wary if someone is recommending you cut out whole food groups or banish gluten or sugar. It’s rarely as simple as that and you can be unnecessarily avoiding foods that are highly nutritious and pleasurable.
5. Move your Body.
Even light activity stimulates digestion and can help release trapped gas. A 10–15 minute walk after meals has been shown to reduce bloating and promote regularity.
6. Manage Stress
Stress activates your “fight or flight” mode, which slows digestion. Over time, this can worsen bloating. Try:
- Deep breathing – Inhale slowly through your nose, exhale through your mouth, focusing on expanding and relaxing your belly.
- Meditation – Even 5 minutes of focusing on your breath can calm your nervous system.
- Mindful eating – Slow down, savor each bite, notice flavors and textures. This helps digestion and prevents swallowing excess air.
7. Will HRT help with bloating?

Hormone Replacement Therapy(HRT)or more correctly called Menopause Hormone Therapy(MHT) is often a game-changer for many menopause symptoms, but bloating isn’t usually one of them. In fact, studies suggest that oral HRT can slow digestion even further, which may not help if bloating is already an issue.
8. Over-the-Counter(OTC) Medications to help with boating:
Short-term relief can come from:
- Antacids (Tums, Rolaids, Maalox) – For bloating linked to indigestion or acid reflux.
- Simethicone (Gas-X, Phazyme, Ovol) – Breaks up gas bubbles.
- Digestive enzymes – Helps break down carbs, fats, and proteins.
- Lactase supplements – For lactose intolerance.
These don’t fix the cause, but can be helpful tools in your kit.
9. Natural remedies for perimenopause bloating:
- Peppermint – Relaxes digestive muscles. Try tea or enteric-coated capsules.
- Ginger – Stimulates digestion; add fresh to meals, sip as tea, or take as a supplement.
- Chamomile – Soothes the gut and reduces inflammation.
- Fennel – Chew seeds or drink as tea to ease gas.
- Probiotics – Support a healthy gut microbiome (think yogurt, kefir, sauerkraut, kimchi. Alternatively, you can take probiotic supplements containing Lactobacillus acidophilus or Bifidobacterium lactis.
When to seek medical help:

Bloating is common during the menopause transition, but that doesn’t mean you should ignore it — especially if it’s persistent, disruptive, or accompanied by other symptoms. Your body has its own way of letting you know when something’s not right, and it’s worth listening.
Book an appointment with your healthcare provider if you notice:
- Bloating that doesn’t improve after trying self-care strategies
- Severe or worsening abdominal pain
- Constipation lasting more than three months
- Unexplained weight loss
- Loss of appetite
- Persistent nausea or vomiting
- Ongoing joint pain
Why a check-up matters
These symptoms could point to something more than hormonal changes. Your provider can rule out (or diagnose) other conditions that may be behind your bloating, such as:
- SIBO (Small Intestinal Bacterial Overgrowth) – Too many bacteria in the small intestine can trigger bloating, gas, and discomfort. A simple breath test can help diagnose it.
- IBS (Irritable Bowel Syndrome) – Causes abdominal pain and changes in bowel habits. Symptoms can worsen during menopause.
- GERD (Gastroesophageal Reflux Disease) – Stomach contents flow back into the esophagus, increasing belching and bloating.
- Celiac disease – An autoimmune reaction to gluten that damages the small intestine lining (villi), interfering with nutrient absorption.
See: Menopause and Heartburn: How to find relief
Menopause bloating is frustrating, yes — but it’s also common, and often manageable once you know what’s driving it. It can be triggered by many things: dietary choices, food intolerances, hormonal shifts, gastrointestinal conditions, even stress.
The key is to play detective and get to the root cause. That’s where you’ll find the most effective, lasting relief. Sometimes it’s as simple as adjusting your diet or daily habits; other times, it means partnering with your healthcare provider to rule out underlying conditions.
And remember — you don’t have to figure it out alone. A registered dietitian can help you identify triggers, fine-tune your nutrition, and find strategies that work for your body in this stage of life.
Your body is changing, yes, but with the right approach, you can feel more comfortable, less bloated, and more in tune with what it needs now.
Curious about other gut issues in menopause? Check out: What the Heck is Going on With My Gut

Looking for ongoing support around food, body, and menopause?

Hi, I’m Sandra!
I’m a registered dietitian and body confidence coach specializing in midlife health and menopause nutrition.
I help women thrive by moving away from restriction and toward nourishment—through practical strategies and compassionate support that honor your changing body.
My focus is on helping you feel confident, strong, and well-fed.
Learn more