Menopause & Diarrhea: Causes, Remedies & Prevention Tips
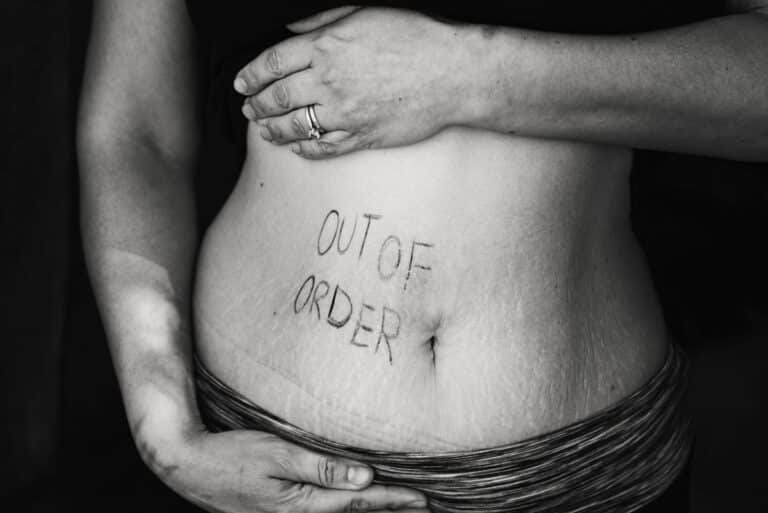
While most people are familiar with common menopause symptoms such as hot flashes and mood swings, there's one symptom that often goes under the radar: diarrhea.
Yes, you read that right! Diarrhea can be an unexpected and bothersome companion during menopause, causing discomfort and disrupting daily routines.
Let’s delve into the connection between menopause and diarrhea, figure out why it might be happening and more importantly what to do about it.

What is diarrhea?
According to the Canadian Society of Intestinal Research diarrhea is defined as the frequent passage of watery, loose stools, accompanied by an excessive loss of fluid and electrolytes. Generally, this means passing more than three liquid bowel movements daily.
Causes of diarrhea during menopause:
Let’s look at some of the key reasons why menopause might be sending you running to the bathroom.
Hormonal fluctuations:

Hormones like estrogen and progesterone play a role in just about everything—including your gut. During menopause, these hormones can fluctuate wildly, and that can throw your digestive system out of whack.
If you ever experienced the so-called “period poops” before your monthly cycle, you’ll know exactly what I mean.
That same fluctuations in estrogen and progesterone that happened premenstrually is happening now—just less predictably—and it can lead to similar symptoms.
Estrogen, in particular, has a strong influence on the gastrointestinal tract. It affects how quickly food moves through your system (gut motility), how sensitive your gut is, and even how inflamed it gets.
So when estrogen levels shift during menopause, it can disrupt your digestion—and diarrhea may be one of the results.
Changes in gut bacteria:

Your gut microbiome—the community of bacteria living in your digestive tract—can also change during menopause.
These shifts can upset the balance of “good” and “bad” bacteria, which may lead to a whole host of digestive issues, diarrhea included.
Stress and anxiety:
Menopause and stress often go hand in hand (hello, 3 a.m. worry sessions). But stress doesn’t just mess with your mood—it can affect your gut, too.
In fact, one study showed that stress is linked to more severe diarrhea in menopausal women. That lines up with what we know from other research: stress increases something called GI permeability, which makes your gut lining more “leaky” and can lead to diarrhea.
Medications and hormone replacement therapy(HRT):

If you're taking medications to manage menopause—especially hormone replacement therapy—digestive side effects like diarrhea may show up.
HRT is meant to ease menopausal symptoms by boosting estrogen and progesterone levels, but it doesn’t always play nice with your gut. For some women, this means new or worsening digestive issues.
Food Sensitivities and Intolerances:
Menopause can affect how your body responds to certain foods. Changes in gut permeability may make you more sensitive to things that never bothered you before.
Dairy (lactose), artificial sweeteners like mannitol or sorbitol, and even alcohol can suddenly trigger digestive symptoms—including diarrhea.
Inflammatory Bowel Syndrome (IBS):

Menopause doesn’t cause IBS directly, but it can stir up symptoms in people who already have it—or who are prone to it.
IBS involves abdominal pain, bloating, and unpredictable bowel habits, and hormonal changes may be a trigger for flare-ups.
The connection isn’t fully understood, and it varies from person to person, but if you’ve noticed your IBS symptoms getting worse during menopause, you’re not alone.
How can I stop menopausal diarrhea?
If your gut has gone rogue during menopause, it can feel devastating.
The good news?
There are plenty of strategies you can try to help get things back on track. Let’s walk through them.

1. Add Soluble Fiber
Soluble fiber is your friend here. It helps bulk up stool by absorbing water in the gut, forming a gel-like consistency that slows things down.
It also acts as a prebiotic, feeding the good bacteria in your gut. These bacteria ferment the fiber and produce short-chain fatty acids—compounds that help nourish the gut lining and support overall gut health.
Foods rich in soluble fiber include:
- Oats and barley
- Legumes like lentils and beans
- Fruits such as pears, apricots, and avocado
- Vegetables like carrots, sweet potatoes, and green peas
- Chia seeds
Start low and go slow. When adding more fiber to your diet, do it gradually to avoid making symptoms worse.
Digestive Symptom Tracker for Midlife Women
A simple tool to help you spot patterns, uncover
triggers, and feel better in your body.
Start tracking today and finally feel in control.
2. Eliminate Food Triggers
Your digestive system might suddenly be reacting to foods you used to tolerate just fine. Welcome to midlife.
Tracking your food and symptoms in a diary for a week or two can help uncover patterns. Common culprits include:
- Lactose (found in dairy)
- Fructose (in fruit and some sweeteners)
- Sugar alcohols like sorbitol and mannitol
- Fatty foods
- Alcohol
If eliminating these doesn't help, you might want to look into a FODMAP-lite approach.
3. FODMAP lite diet:
You may have heard of the FODMAP diet—a highly structured eating plan used to manage IBS and other gut issues. FODMAPs are types of carbohydrates that can ferment in your colon and cause symptoms like bloating, gas, and diarrhea.
The full version of this diet is pretty restrictive and best done with a dietitian. But a gentler version, sometimes called FODMAP-lite, can be a good starting point.
Try reducing only the highest FODMAP offenders, such as:
- Wheat and rye
- Lactose-containing dairy
- Legumes
- Certain fruits like apples, pears, stone fruits, watermelon, and dried fruit
- Certain vegetables like onion, leek, cauliflower, and mushrooms
If symptoms improve after avoiding these foods, begin reintroducing them one at a time to see which ones are actually triggering your symptoms.
Pro tip: A registered dietitian can make this process a whole lot easier—and ensure you’re not missing key nutrients if you need to stay off certain foods long-term.
4. Stay hydrated
This one’s simple but crucial: drink enough fluids. Diarrhea can quickly lead to dehydration, especially if it’s happening frequently.
Aim for water, herbal teas, or infused waters (think cucumber-mint or lemon-ginger). Avoid overdoing it with caffeine and sugary drinks—they can make things worse.
5. Stress management

Stress and digestion are deeply connected—and menopause often brings a spike in both stress and anxiety, thanks to shifting cortisol levels. (Or shifting everything!)
Try adding simple stress-reducing practices into your daily routine, such as:
- Deep breathing or mindfulness meditation
- Gentle yoga or stretching
- Walking or light exercise
- Creative hobbies that calm the nervous system
Small daily habits can make a big difference.
6. Consider Probiotics
Probiotics are beneficial bacteria that help keep your gut ecosystem in balance. They can sometimes help with regulating digestion and easing diarrhea.
You can find probiotics in foods like:
- Yogurt (look for “live and active cultures”)
- Kefir
- Sauerkraut and kimchi
You might also try a probiotic supplement, but keep in mind:
- Not all strains work the same way
- What works for one person may not work for another
- It may take some trial and error to find the right fit
7. Over the counter medications

For short-term relief, these can be helpful:
- Imodium (loperamide): Helps slow down bowel movements
- Pepto-Bismol or Kaopectate (bismuth subsalicylate): Can reduce diarrhea and soothe the stomach
Psyllium husk (like Metamucil) is another option. It’s a soluble fiber supplement that can help firm up loose stools.
Try starting with 5 grams once or twice a day, mixed with water or juice—and make sure to drink extra fluids when using it.
None of these strategies are one-size-fits-all, and it may take some experimenting to find what works best for your body.
But with a little patience (and possibly a supportive health professional in your corner), you can definitely get a handle on menopausal diarrhea.
When should I seek help?

Menopausal diarrhea can be frustrating, exhausting, and sometimes even a little alarming. While some digestive changes during menopause are normal, ongoing or severe diarrhea is not something you should just put up with.
It’s time to check in with your healthcare provider if:
- The diarrhea persists beyond a few days or weeks
- It starts to interfere with your daily life or sleep
- You notice additional symptoms like:
- High fever
- Severe abdominal pain
- Signs of dehydration (e.g., excessive thirst, dry mouth, dark urine)
- Blood in your stool
Every woman’s experience with menopause is different—and that includes how your gut behaves during this transition.
If you’re suddenly dealing with unpredictable bathroom habits or foods that no longer seem to agree with you, there’s nothing unusual about that. It’s a common (but rarely talked about) part of midlife.
The encouraging part? There are ways to manage it. Making small shifts in your diet, dialing down stress and getting support when needed—these are all solidsteps that can make a real difference.
It might take a bit of experimenting, but you don’t have to settle for living in discomfort.
Think of this as a chance to reconnect with your body in a new way—and give your digestive system the care and attention it’s been asking for.
Curious about other gut issues in menopause? Check out: What the Heck is Going on With My Gut.

Looking for ongoing support around food, body, and menopause?

Hi, I’m Sandra!
I’m a registered dietitian and body confidence coach specializing in midlife health and menopause nutrition.
I offer virtual nutrition counselling and coaching for women in British Columbia, Canada.
I help women thrive by moving away from restriction and toward nourishment—through practical strategies and compassionate support that honor your changing body.
My focus is on helping you feel confident, strong, and well-fed.
Learn more about working with me